Phase 1 – MD Curriculum
Phase 1 of the ForWard Curriculum focuses on basic science while fully integrating clinical science and all curriculum threads. This phase is completed within 18 months of starting medical school. A primary feature of Phase 1 is small group case-based learning through Patient-Centered Education (PaCE) Cases.
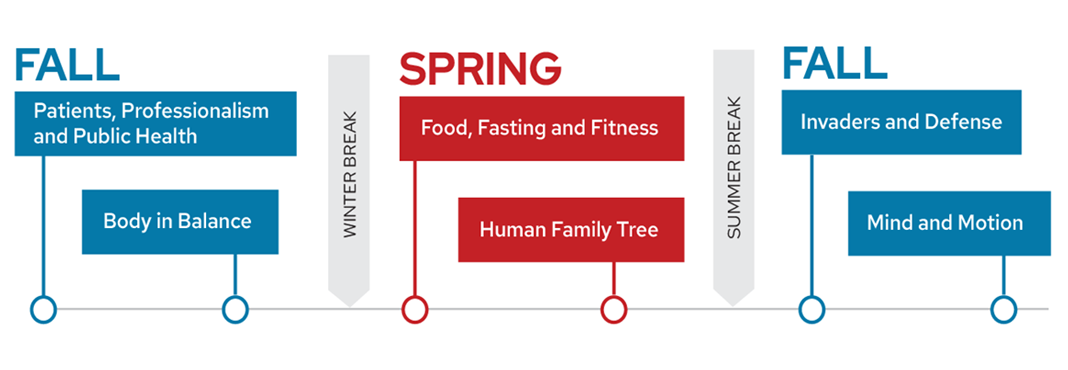
Phase 1 Timeline
Phase 1 Blocks
Patients, Professionalism and Public Health
Patients, Professionalism and Public Health establishes a strong foundation for a student’s professional identity formation as a physician. The course begins with “Faces of Patients,” where you see the impact of illness on the lives of patients and their loved ones. The concept of patient-centered care is introduced and practiced through real and standardized patient interviews. You will be asked to look beyond immediate measures of health toward the many upstream determinants of health that impact your patients’ lives.
You are introduced to the concept of health equity, which is the goal of providing everyone a fair shot at being as healthy as possible. You will learn how racism, bias and structural inequities threaten that goal, and ways you as a physician can work to overcome those obstacles. You will explore how patients’ culture impacts their health and how the social history can illuminate those factors during the medical interview.
You consider the various health-related systems that can impact a person’s health and illness, including their community, the health care system, the public health systems and the role of quality improvement. Students see how effective health care can only be delivered by working as a part of an interdisciplinary team.
Finally, you will contemplate the importance of each individual physician in health promotion. Your first encounter with human anatomy as a medical student allows further exploration of the sacred role of physician and the unique privilege and responsibilities of the profession. The course ends with “Faces of Physicians,” where you will delve into the myriad ways that physicians can advocate for health, whether it be for a single patient or for an entire population.
Course Objectives
- Demonstrate basic observation skills to locate and describe the organization of the human body
- Describe key concepts in cell function and damage, excitable membranes and cell signaling
- Describe key concepts in and mechanisms of genetic inheritance
- Demonstrate basic communications skills with patients in the context of the medical interview
- Describe the principles of interprofessional collaboration and demonstrate basic communication and team skills in interprofessional team settings
- Describe skills that can promote health equity in patient-doctor interactions
- Describe the major aspects of the immune response to injury and infection
- Discuss and describe mechanisms related to foundational basic science concepts in patient-centered cases
- Describe the role of scientific inquiry in medicine and integrate new knowledge with peers to promote learning and retention
- Describe basic concepts related to public health, population health, and social determinants of health
- Describe the main categories of infectious diseases and common mechanisms for causing human illness
- Demonstrate an understanding of the basic structure and function of the nervous system
- Obtain the chief concern, history of present illness, past medical history, family history and social history
- Describe and apply basic concepts related to epidemiology and evidence-based medicine
- Use self assessment and feedback to improve your skills and the skills of others
- Demonstrate behaviors that contribute to constructive group dynamics and an environment of discovery
- Demonstrate respect and non judgmental behavior towards peers, patients and teachers and honor the personal stories that patients share
- Take responsibility and demonstrate timely, organized and dependable behavior
- Describe basic principles of medical ethics and patient confidentiality
- Describe the principles of community engagement and advocacy for patients and populations
- Describe the signs of opioid intoxication and the risk factors for developing an opioid use disorder
- Describe basic principles of patient safety and quality improvement
- Describe key components of health care systems and principles for evaluating health care delivery
Body in Balance
Body in Balance covers the key processes involved in maintaining internal balance in the body. In this course, you will follow the path of the red blood cell and will pause to review normal function and disease at each step of the journey.
You will begin with the birth of the red blood cell in the bone marrow and a discussion of anemia. Then there will be an introduction to the processes involved in bleeding and clotting followed by a discussion of hemostatic and thrombotic disorders. Following our red blood cell through the circulation, you will stop to review the mechanical and electrical functions of the heart and will learn about the dynamic control of vascular function, along with the importance of the lymphatic system.
Atherosclerosis is introduced as the underlying process of cardiovascular disease, and the rupture of a coronary plaque allows for you to see the clotting cascade in action. We then find our red blood cell in a heart that has gone awry. You will discuss etiologies and treatments of electrical disturbances, cardiac inflammatory diseases, valvular dysfunction and heart failure.
Next, you will follow our red blood cell as it travels through the pulmonary circulation, where it participates in gas exchange as you review lung function and common lung diseases.
The final stop on the circulatory tour is through the kidneys, which function in waste disposal as well as regulation of hemodynamics, water and electrolyte balance, and acid/base status. The close coordination of the cardiovascular and renal systems as long-term regulators of blood pressure is highlighted via discussion of congestive heart failure and hypertension. The course closes with a discussion of various causes and manifestations of renal dysfunction.
Examples of integrated longitudinal threads include a discussion of the ethics and stewardship of transplantation in chronic kidney disease, randomized controlled trials involving treatments in stroke prevention, and environmental health and its impact on disease states such as obstructive lung disease.
Course Objectives
- Describe basic principles of enzymes including enzyme kinetics and inhibitors
- Describe the normal structure and function of the cardiovascular system as well as the underlying pathologic processes, clinical features, and management of cardiovascular disorders
- Explain endocrine involvement in the cardiovascular and renal systems, including functions of vasopressin/ADH, aldosterone, epinephrine, and parathyroid hormone in normal and disease states
- Describe the genetics involved in various anemias and bleeding disorders
- Describe the role of the gastrointestinal system in the development of pernicious anemia and symptoms of cystic fibrosis
- Describe hematopoiesis, normal red blood cell biology, composition, and function, and normal platelet biology including the roles of platelets in hemostasis and thrombosis, and describe the underlying pathologic processes, clinical features, and management of anemias as well as various thrombotic and bleeding disorders
- Participate as a student in a care team and effectively explain your role to patients and families
- Explore the importance of diverse roles and perspectives on clinical teams in both simulated and clinical environments
- Explore various examples of how the social determinants of health affect individuals, families, and communities, thus contributing to health disparities and structural racism
- Effectively convey clinical information in written and oral forms with a focus on cardiovascular and pulmonary concerns
- Describe the basic principles of the complement cascade
- Discuss and describe mechanisms related to foundational basic science concepts in patient-centered cases
- Analyze and critique study design and interpretation in clinical and translational research, analyze biostatistics reported in clinical trials, and critically evaluate scientific literature to deepen understanding of a clinical scenario
- Integrate the role of social, environmental, and structural determinants of health on health promotion, health equity, and prevention of sickle-cell anemia, cardiovascular disease, asthma, and chronic kidney disease
- Describe the normal structure and function of the renal system including normal acid-base balance and the normal handling of water and electrolytes, and describe the underlying pathologic processes, clinical features, and management of renal disorders, acid-base disturbances, and electrolyte imbalances
- Describe the general organization, structure, and function of the autonomic nervous system including innervation of organs of the cardiovascular, respiratory, and renal systems
- Acquire and synthesize relevant patient information and diagnostic test results related to cardiovascular, pulmonary, and nephrology systems to formulate an appropriate differential diagnosis and patient-centered care plan
- Counsel patients about the importance of smoking cessation on disease prevention and educate patients on available resources for smoking cessation
- Describe basic principles of pharmacology and pharmacokinetics
- Integrate concepts across multiple domains using guided inquiry to identify gaps in knowledge and to find appropriate resources to address medical and public health questions
- Identify areas for personal improvement of knowledge, skills, and attitudes, and set goals to affect change in those areas, tracking progress toward attainment of goals
- Engage in self directed learning, share knowledge gained with members of the professional community, and demonstrate effective methods for giving and receiving feedback
- Demonstrate respect and non judgmental behavior towards peers, patients, and teachers and honor the personal stories that patients share
- Participate reliably and conscientiously in group learning settings and when working with patients
- Discuss ethical issues in the setting of human-studies research and explain the ethical implications of rationing
- Identify community-level support systems as well as the physician role in addressing disparities in CKD screening, treatment, and outcomes
- Describe the normal structure and function of the respiratory system as well as the underlying pathologic processes, clinical features, and management of respiratory disorders
- Reflect on the impact of careful history taking and exam on patient safety and recognize the importance of observing impact of quality improvement on health care delivery over time
- Provide examples and explain outcomes of clinical practices and public health programs that address health inequities and/or aim to reduce detrimental environmental exposures in order to educate and protect patients and populations
- Explain the importance of stewardship and the right of refusal of care in the health care system and describe key concepts related to health care costs and health care payers in the U.S.
Food, Fasting and Fitness
Food, Fasting and Fitness explores the chain of events by which food is converted to energy, highlighting the key role of nutrition and exercise in the maintenance of optimal health. Starting with food on a plate, you will learn the importance of the various macro- and micronutrients and healthy food choices. You will explore the role of nutrition in maintaining the health of individuals as well as the health of communities.
You will learn about the digestive system and the processes that allow food to become nutrients in the bloodstream. The absorption of these nutrients is sensed, prompting endocrine signals that inform cells that nutrients are available for uptake and use. You will learn about these signals and also the cellular biochemical processes involved in the burning and storing of energy by cells.
Following this, you will compare and contrast the fed state with processes that are instituted by the body to allow survival in between meals and with prolonged fasting. Understanding of these mechanisms underpins discussion of the increasing health threat of metabolic disorders such as diabetes, obesity and lipid disorders. You will explore the metabolic changes that occur with exercise and the role of exercise and fitness in good health. Finally, discussion of the removal of waste products and toxins completes an integrated picture of metabolism.
Examples of integrated longitudinal threads include advocacy surrounding nutrition in communities, public health related to impact of climate change on food, use of the electronic medical record and quality improvement in medical care, discussion of health literacy in the setting of diabetes care and exploring fundamental principles of scientific inquiry via critical examination of nutrition guidelines.
Course Objectives
- Describe the role of biochemical pathways in the normal physiology of metabolism, how these pathways are regulated, and the underlying pathologic processes in disorders of metabolism
- Describe the histology and physiology of the endocrine system and describe the underlying pathologic processes, clinical features, prevention, and management of endocrine disorders relating to metabolism, including diabetes, obesity, thyroid disorders, adrenal disorders, and pituitary disorders
- Describe the anatomy, histology, and physiology of the digestive system and describe the underlying pathologic processes, clinical features, prevention, and management of digestive system disorders
- Describe the etiology, clinical manifestation, diagnosis, and management of genetic metabolic disorders and how natural selection has resulted in genetic variation within and among human populations
- Demonstrate effective communication with patients, including skills in motivational interviewing and navigating challenging patient interactions
- Discuss the importance of effective clinical teamwork using care related to nutrition and obesity as an example
- Effectively describes and evaluates evidence-based public health policies
- Discuss the impact of health literacy limitations, socioeconomic disparities, and poverty on health and examine food sovereignty as an example of methods to promote health and health equity
- Effectively convey patient information in written and oral forms, with a focus on abdominal concerns
- Describe the physiologic processes by which the body generates an immune response, inflammation, and autoimmune disease
- Discuss and describe mechanisms related to foundational basic science concepts in patient-centered cases
- Critically evaluate scientific literature to deepen understanding of a clinical scenario
- Discuss social and structural determinants of health, such as poverty, nutrition quality, nutrition access, and climate change, and their impact on metabolic disease risk and prevention, health promotion, and health equity
- Describe physiologic that allow for muscle performance and pathologic processes that result in metabolic disease
- Describe the role of appropriate nutrition, exercise and fitness in health and disease prevention and identify underlying pathologic processes, clinical features, risk factors, prevention, and management of metabolic and malnutrition-related disease including macro- and micro-nutrient deficiency and toxicity
- Acquire and synthesize relevant patient information from history and physical examination in order to formulate an appropriate differential diagnosis and patient-centered care plan for abdominal complaints, gastrointestinal disease, and malnutrition
- Discuss technology use in the care of patients, including optimal use of an EHR
- Apply skills in evidence-based reasoning by asking appropriate clinical questions, locating and appraising evidence, and interpreting biostatistics
- Utilize self-reflection and feedback from peers and instructors to improve your own knowledge, skills and attitudes and to facilitate group learning
- Engage in self directed learning, share knowledge gained with members of the professional community, and demonstrate effective methods for giving and receiving feedback
- Demonstrate respect and non judgmental behavior towards peers, patients and teachers and honor the personal stories that patients share
- Demonstrate responsibility by being organized and dependable while working with peers
- Participate reliably and conscientiously in group learning settings
- Apply principles of informed consent to a patient scenario
- Serve as an advocate and practice the key principles of community engagement to promote nutrition access and metabolic health of patients and populations
- Describe the major classes of pharmacologic therapies for lipid disorders, diabetes, thyroid disorders, and other metabolic diseases, and describe mechanisms of drug metabolism and toxicity and related management of drug toxicities and poisonings
- Demonstrate understanding of quality improvement processes to optimizes quality and prioritize patient safety measures
- Discuss health policy approaches to improve nutrition and wellness for patients and populations, including those experiencing poverty
- Evaluate health care costs, quality of life, and cost-effectiveness measures to optimize quality care for patients and populations and demonstrate best utilization of health care resources
Human Family Tree
Imagine that you are a new family medicine physician in a busy practice. Your 11 o’clock appointment is a young couple that recently moved to town. The couple wishes to establish a primary care medical home with you. During the visit, they inform you that they are hoping to start a family soon. Human Family Tree will follow your journey with this couple and their family, through the remainder of their life cycle.
You will explore the molecular, genetic, embryologic, hormonal, anatomical, and physiological factors that govern fertility, cell growth, fetal development, and pregnancy, as well as the congenital anomalies that can occur when those processes are aberrant.
Your journey with the family will continue through the birth of their child, when you will discuss lactation and newborn screening while later exploring childhood growth and development. You will grapple with difficult issues that can affect families such as domestic and child abuse. You will follow their child’s development into young adulthood and learn about the biological basis of puberty and discuss issues affecting adolescents and young adults. You will explore concepts important to ensuring inclusive and equitable treatment of those who identify as part of the LGBTQ+ community.
You will explore the genetic basis of human disease and how to screen the family for conditions that might impact their health and/or reproductive risk. You will learn about the hormonal and physiological changes in reproductive health with menopause and aging. You will also learn about the consequences of unregulated cell growth (cancer) to your patient and their family. And finally, you will support the family through end-of-life issues brought on by cancer in a family member.
Examples of integrated longitudinal threads include evidence-based medicine and health policy related to fertility treatments, health disparities in cancer prevention/screening, and reproductive ethics.
Course Objectives
- Review key features of the anatomy and physiological functions of the cardiovascular system and compare with fetal circulation
- Describe the clinical features, diagnosis, and management of congenital heart diseases
- Describe pathophysiology of congenital heart disease
- Describe the normal physiology of childhood growth, development, and puberty
- Describe the clinical features, diagnosis, and management of disorders of childhood growth and puberty
- Describe the pathophysiology of disorders affecting childhood growth and puberty
- Describe fertilization as well as the embryological development of the major organ systems, gametes, embryos, and fetuses, and explain the importance of development on human physiological and pathophysiological states
- Describe important anatomic features of the abdominal wall and inguinal canal
- Describe the heredity and genetic variation of inherited characteristics in human development, how genetics impacts human physiological and pathophysiological states, and management strategies for genetic disorders
- Describe the heredity and genetic variation of inherited characteristics in human development, how genetics impacts human physiological and pathophysiological states, and management strategies for genetic disorders
- Use patient-centered language when communicating patients and families about sensitive topics including regarding sexual history and gender identity as well as during GU, gynecologic, and pelvic examinations
- Identify and apply skills that facilitate collaborative, team-based care in a clinical setting
- Effectively convey evidence-based health practices, programs, and policies using media, written, or oral platforms
- Describe means of addressing health inequities faced by populations such as children, adolescents, and the LGBTQ+ community
- Effectively convey patient information in written and oral forms, with a focus on reproductive endocrinology concerns
- Describe key features of sexually transmitted infections
- Discuss and describe mechanisms related to foundational basic science concepts in patient-centered cases
- Critically evaluate scientific literature to deepen understanding of a clinical scenario
- Explore the role of social and structural determinates of health on equity of outcomes in parental/child health and elderly populations
- Identify and describe the anatomy and physiological functions of the lower urinary system
- Describe the clinical features, diagnosis, and management of disorders of the lower urinary tract
- Describe the disordered physiological processes of the lower urinary tract
- Identify and describe the and embryological features of the cranial nerves
- Describe clinical features related to developmental disabilities as well as disability and loss of capacity with aging
- Describe the components of breastmilk and formula, why these nutrients are needed for growth and development, and ways to provide these nutrients to the newborn
- Describe the clinical features, diagnosis, and management of solid cancers of the major organ systems as well as risk factors, epidemiology, and prognosis of these cancers
- Identify characteristics of solid cancers of major organs under microscopic examination in order to study these pathologic processes
- Describe the disordered physiological processes of solid cancers of the major organ systems
- Describe the mechanism of action and use of medications used in the management of solid cancers of the major organ systems
- Acquire and synthesize relevant patient information to formulate an appropriate differential diagnosis and patient-centered care plan related to a patient’s reproductive and GU health and discuss issues of autonomy in the aging patient
- Practice the use of the electronic health record in a simulated setting
- Engage in evidence-based reasoning and problem solving to address medical and public health questions related to genetics, reproduction, and cancer
- Utilize self-reflection and feedback from peers and instructors to improve your own knowledge, skills and attitudes and to facilitate group learning
- Engage in self directed learning, share knowledge gained with members of the professional community, and demonstrate effective methods for giving and receiving feedback
- Demonstrate respect and non-judgmental behavior towards peers, patients and teachers and honor the personal stories that patients share
- Participate reliably and conscientiously in group learning settings
- Discuss key ethical principles relating to vulnerable patients and populations, including children, adolescents, elders, and those that are pregnant or at risk for domestic violence
- Describe and demonstrate skills of community engagement and advocacy to promote patient and population health
- Describe the clinical features, diagnosis, and management of respiratory distress syndrome in the neonate
- Identify and describe the anatomy and physiological functions of the major reproductive organ systems
- Describe the clinical features, diagnosis, and management of both physiological functions and diseases of the major reproductive organ systems as well as risk factors, epidemiology, and prognosis of reproductive organ system disorders and diseases
- Identify tissues of the reproductive organs under microscopic examination in order to study their physiological and pathophysiological characteristics
- Describe the disordered physiological processes of the organs of the reproductive system that cause, result from, or are associated with disease or injury
- Describe the mechanism of action and use of medications used in the management of diseases of the reproductive organ system
- Identify and explain systems in place to manage both quality and safety in an ambulatory clinic
- Describe individual and population-based strategies to improve health outcomes for vulnerable populations including children/adolescents, pregnant individuals, and those at risk for domestic violence
Invaders and Defense
Invaders and Defense covers material in the areas of microbiology, immunology, infectious disease, autoimmune disease, hematologic malignancy and dermatologic disease. You will first learn about the “foot soldiers” of innate immunity — those charged with handling routine invasions and threats, followed by the “special forces” of the adaptive immune system. The importance of the integumentary system as the “coast guard” will be discussed, with study of normal skin function and dermatologic pathology, infectious, inflammatory and neoplastic.
You will discuss the nature and clinical manifestations of the various types of biological invaders (bacteria, viruses, fungi and parasites), the clinical syndromes that they are associated with and mechanisms used to fight these infections.
The analogy continues to be helpful to understand the concepts of immune deficiency — where one or more elements of the normal defense system break down (or is purposely suppressed, such as in transplantation) — as well as autoimmunity, where normal tissues are attacked and damaged due to “bad intel” and “friendly fire.” Hematology malignancy presents as a “coup” — when some element of the immune system ceases to function within its role and overtakes and destroys normal immune function.
Examples of integrated longitudinal threads include shared decision-making and autonomy, focusing on the legal, ethical and public health aspects of vaccination. Clinical skills include oral reporting and the head and neck physical exam.
Course Objectives
- Apply knowledge of skin structure and function, innate and adaptive immunity, and microbiology to the explain the mechanisms, clinical and laboratory findings, and treatments of dermatologic disorders and neoplasia
- Describe normal anatomy as relevant to the nasal passages and sinuses
- Apply knowledge of the molecular basis of neoplasia to explain of the biological behavior, morphologic appearance, classification, diagnosis, prognosis, and targeted therapy of hematologic neoplasms
- Explain the key concepts related to shared medical decision-making.
- Demonstrates effective communication and team skills to establish and maintain collaborative relationships with members of the interprofessional team
- Identify issues related to bias and stereotyping that lead to health care inequities
- Effectively communicate patient information in written and oral formats
- Apply basic knowledge of pathogenic and commensal microorganisms to explain the biologic mechanisms, clinical and laboratory features, and potential therapeutic approaches to infectious diseases and syndromes
- Apply knowledge of the normal immune system to promote microbial defense, repair of injury, and to understand the biologic mechanisms, clinical lab features, and therapeutics for autoimmune disorders
- Discuss and describe mechanisms related to foundational basic science concepts in patient-centered cases
- Identify, analyze and apply emerging research related to molecular diagnostics
- Discuss key concepts of public health and health equity relating to infectious diseases prevention and outcomes
- Identify pathogenic microorganisms including the fundamental mechanisms of their pathogenicity
- Acquire and synthesize relevant patient information to formulate an appropriate differential diagnosis and patient-centered care plan
- Use an Electronic Health Record (EHR) for patient care
- Demonstrate skills in evidence-based medicine, including the ability to effectively search for evidence and interpret randomized controlled trials
- Utilize self-assessment and feedback from multiple sources to improve knowledge, skills and attitudes
- Contribute to an environment of discovery and learning as a member of a professional community
- Respect human dignity and diversity by demonstrating accepting, non-judgmental behaviors and providing compassionate care for all
- Demonstrate responsibility by being organized and dependable while working with peers
- Discuss ethical issues in the setting of human-studies research as well as those surrounding governmental powers, individual autonomy, and the population good.
- Discuss mechanism of action, use and adverse effects of medications used in therapy of dermatologic, infectious and rheumatologic disorders and hematologic malignancies
- Identify and explain systems in place to manage both quality and safety in an ambulatory clinic
Mind and Motion
The final Phase 1 block, Mind and Motion, brings together concepts in musculoskeletal, neurologic, ophthalmologic, and psychiatric medicine as well as basic science domains of anatomy, neuroscience, neuroanatomy, cell biology, and neuro- and psychopharmacology. This is accomplished through analysis of the structure and functions of the central nervous system, peripheral nervous system and musculoskeletal system, as well as study of the disease processes that affect these systems.
The course will begin with an exploration of normal behavioral process and common psychiatric disorders including well-defined diagnostic criteria, use of the psychiatric interview to elicit signs and symptoms, and various therapies.
You will then shift your focus to the spinal column, spinal cord, brain, skull base, intracranial vessels and special senses. In this neurology course component, you will explore how lesions at specific locations along the neuraxis result in predictable neurologic symptoms for pathologic conditions including stroke, multiple sclerosis, trauma, intracranial hemorrhage, tumors and CNS infections, to name a few. The structure and electrical functions of neurons will be discussed, as well as their complex assembly into the brain and spinal cord nuclei and tracts.
Finally, you will explore several common musculoskeletal conditions (fractures, osteoarthritis, a variety of sports injuries, joint pain and nerve entrapment syndromes, among others). Through these common patient presentations, you will develop an understanding of limb anatomy and the specialized tissues of bone, muscle, tendon/ligament, cartilage and nerve.
Examples of integrated longitudinal threads include the ethics of informed consent and conflicts of interest in interactions with industry, in addition to cultural humility, determinants of health care cost, appraising evidence, quality improvement and interprofessional education.
Course Objectives
- Review the concept of hypovolemic shock in the setting of trauma
- Describe the normal hormonal regulation and common disorders of mineral metabolism
- Demonstrate effective communication to establish collaborative relationships with patients and families using in-person and telehealth interview best practices
- Discuss the importance of effective interprofessional clinical teamwork using psychological care and rehabilitation care as examples
- Discuss how the interplay between social inequities and ideas about race, class, and gender can impact patient care and health care policy
- Effectively convey patient information in oral and written forms, with a focus on neurological and musculoskeletal concerns
- Describe key clinical features of infections of the central nervous system
- Discuss and describe mechanisms related to foundational basic science concepts in patient-centered cases
- Critically evaluate scientific literature to deepen understanding of a clinical scenario
- Recognize the public health impact of access to mental health care, over-prescription of opioid pain medications, and macro- and micro- economic determinants of health care
- Describe the anatomy and physiology of the musculoskeletal system and discuss the clinical presentation, diagnosis and management of various neurologic disorders
- Describe the anatomy and physiology of the central and peripheral nervous system and discuss the clinical presentation, diagnosis and management of various neurologic disorders
- Acquire and synthesize relevant patient information to formulate an appropriate differential diagnosis and patient-centered care plan for psychiatric, neurologic and musculoskeletal disorders
- Describe EHR and Telehealth best practices while caring for patients
- Engage in evidence-based reasoning and problem solving and describe the role of systematic reviews as evidence to guide decision-making
- Utilize self-reflection and feedback from peers and instructors to improve your own knowledge, skills and attitudes and to facilitate group learning
- Engage in self directed learning, share knowledge gained with members of the professional community, and demonstrate effective methods for giving and receiving feedback
- Demonstrate respect and non judgmental behavior towards peers, patients and teachers and honor the personal stories that patients share
- Participate reliably and conscientiously in group learning settings
- Discuss the ethics of informed consent and of physician interaction with industry
- Describe the functions of the brain regulating psychologic functioning and discuss the clinical presentation, diagnosis, and management of various psychiatric conditions
- Discuss health care financing and the economic factors that impact care of individual patients and communities